Inflammatory Bowel Disease
Treatments
Inflammatory Bowel Disease
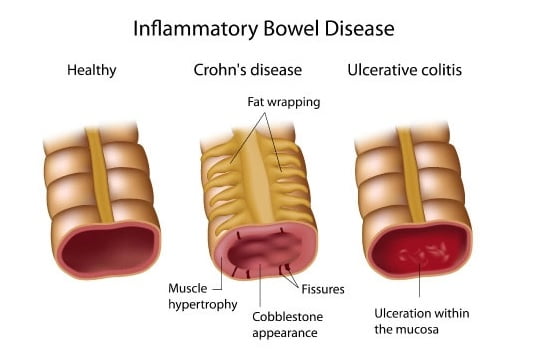
Inflammatory bowel disease (IBD) refers to a group of chronic inflammatory conditions that affect the gastrointestinal (GI) tract. The two main types of IBD are Crohn's disease and ulcerative colitis. These conditions are characterized by periods of inflammation and damage to the digestive tract, leading to various symptoms and complications.
Crohn's Disease
Location
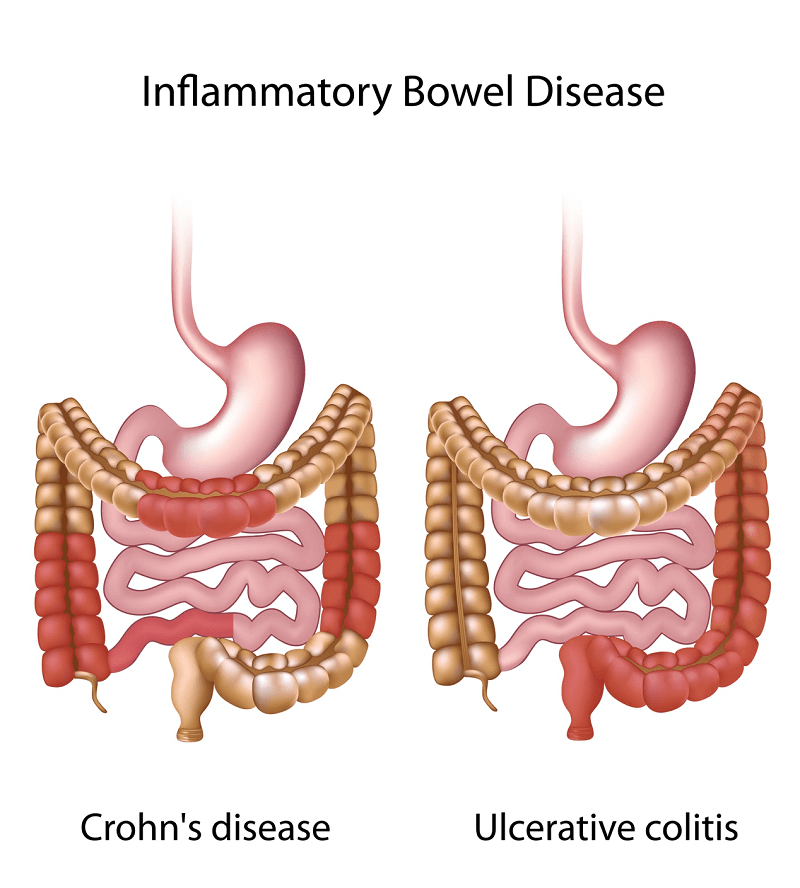
Can affect any part of the digestive tract, from the mouth to the anus, but most commonly involves the end of the small intestine (ileum) and the beginning of the large intestine (colon).
Inflammation
Inflammation can occur in all layers of the intestinal wall and can be patchy, with normal areas of intestine between inflamed ones.
Symptoms
Symptoms vary widely and may include abdominal pain, diarrhea (sometimes bloody), weight loss, fatigue, fever, and complications such as fistulas, abscesses, and strictures.
Complications
Crohn's disease can lead to complications such as bowel obstruction, malnutrition, intestinal perforation, and the development of perianal disease (e.g., fistulas or abscesses).
Ulcerative Colitis
Location
Primarily affects the colon and rectum, with continuous inflammation starting from the rectum and extending into the colon in a continuous manner.
Inflammation
Inflammation is typically limited to the innermost lining (mucosa) of the colon and rectum.
Symptoms
Common symptoms include bloody diarrhea, abdominal pain, urgency to defecate, weight loss, fatigue, and complications such as severe bleeding, toxic megacolon, and increased risk of colon cancer.
Complications
Long-term complications of ulcerative colitis include an increased risk of colon cancer, as well as extraintestinal manifestations affecting other organs, such as the skin, joints, and eyes.
Treatment

Medications
Anti-inflammatory drugs (e.g., corticosteroids, mesalamine), immunosuppressants (e.g., azathioprine, methotrexate), biologic therapies (e.g., anti-TNF agents, integrin antagonists), and antibiotics may be prescribed to control inflammation, manage symptoms, and induce and maintain remission.

Nutritional Therapy
Nutritional supplementation or dietary modifications may be recommended to address nutritional deficiencies, manage symptoms, and promote healing of the digestive tract.

Surgery
Surgery may be necessary in cases of severe complications, refractory disease, or to remove diseased portions of the intestine (e.g., bowel resection) in Crohn's disease or to cure ulcerative colitis (e.g., total colectomy with ileal pouch-anal anastomosis).

Lifestyle Modifications
Avoiding trigger foods, managing stress, regular exercise, and smoking cessation may help manage symptoms and improve overall health.
Causes
The exact cause of IBD is not fully understood, but it is believed to involve a combination of genetic, environmental, immunological, and microbial factors. Factors that may contribute to the development of IBD include:
Genetic predisposition
Family history of IBD increases the risk.
Dysregulated immune response
The immune system mistakenly attacks the digestive tract.
Environmental factors
Factors such as diet, smoking, infections, and stress may trigger or exacerbate symptoms.
Altered gut microbiota
Changes in the composition of gut bacteria may play a role in the development and progression of IBD.
Diagnosis
Treatment for IBS is aimed at relieving symptoms and improving quality of life. This may involve a combination of lifestyle modifications, dietary changes, medications, and stress management techniques:

Medical History and Physical Examination
Includes evaluation of symptoms, family history, and physical examination of the abdomen.

Endoscopic Procedures
Colonoscopy and sigmoidoscopy allow direct visualization of the colon and rectum to assess the extent and severity of inflammation and to obtain biopsies for histological examination.

Imaging Studies
Imaging tests such as CT scans, MRI, or small bowel series may be used to evaluate the extent of inflammation, detect complications, or monitor disease progression.

Laboratory Tests
Blood tests to assess inflammation (e.g., C-reactive protein, erythrocyte sedimentation rate), anemia, nutritional deficiencies, and markers of immune function may aid in diagnosis and monitoring.