Liver Cirrhosis
Treatments
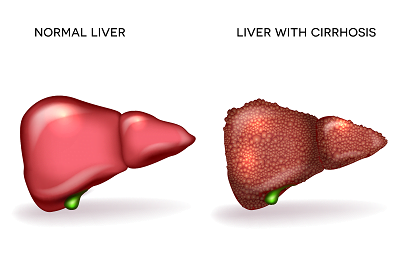
Liver Cirrhosis
Liver cirrhosis is a chronic, progressive liver disease characterized by the replacement of healthy liver tissue with scar tissue, which impairs the liver's ability to function properly. This condition is often the result of long-term liver damage and inflammation. Here's a detailed overview:
Symptoms

Fatigue
Feeling tired and weak is common.

Jaundice
Yellowing of the skin and eyes due to impaired liver function.

Swelling
Fluid retention in the legs and abdomen (ascites) can occur.

Confusion and forgetfulness
Due to toxins not being effectively filtered from the blood (hepatic encephalopathy).

Itchy skin
Due to bile accumulation.

Easy bruising and bleeding
The liver's inability to produce enough clotting factors leads to easy bleeding and bruising.

Weight loss
Loss of appetite and muscle wasting may occur.
Diagnosis
Physical examination:
Includes assessing for signs of liver disease such as jaundice, ascites, and spider-like blood vessels on the skin.
Blood tests:
Liver function tests, complete blood count, and tests for viral hepatitis.
Imaging studies:
Ultrasound, CT scan, or MRI to visualize the liver and assess for signs of cirrhosis.
Liver biopsy:
A sample of liver tissue is taken and examined under a microscope to confirm the diagnosis and assess the extent of liver damage.
Treatment

Address underlying cause
Treatment may involve lifestyle changes (such as quitting alcohol), antiviral medications for hepatitis, or managing conditions like diabetes and obesity.

Medications
Drugs may be prescribed to manage symptoms, improve liver function, or reduce complications (e.g., diuretics for ascites, lactulose for hepatic encephalopathy).

Liver transplant
In advanced cases where liver function is severely compromised, a liver transplant may be necessary.

Complication management
Treatment may also involve managing complications such as variceal bleeding, infections, and nutritional deficiencies.
Causes
Alcohol abuse:
Chronic excessive alcohol consumption is one of the most common causes of cirrhosis.
Viral hepatitis:
Hepatitis B and C viruses can lead to chronic liver inflammation and eventually cirrhosis.
Non-alcoholic fatty liver disease (NAFLD) and non-alcoholic steatohepatitis (NASH):
Obesity, diabetes, and metabolic syndrome can cause fat to accumulate in the liver, leading to inflammation and cirrhosis.
Autoimmune hepatitis:
The body's immune system mistakenly attacks liver cells, leading to inflammation and cirrhosis.
Primary biliary cirrhosis (PBC) and primary sclerosing cholangitis (PSC):
These are autoimmune conditions affecting the bile ducts, leading to liver inflammation and cirrhosis.